When you hear the term “breast cancer survivor,” what comes to mind? For many, it’s the image of crossing a finish line after the last treatment. But the truth is, survivorship isn't a destination—it's a journey that begins the moment you're diagnosed. It’s the entire process of healing, adapting, and rediscovering yourself long after the active fight is over.
What Breast Cancer Survivorship Really Means
The word "survivor" can feel complicated. While it certainly marks a profound victory over the disease, the reality of life after breast cancer is far more layered. Survivorship truly encompasses every single step you take from day one—navigating the shock of diagnosis, enduring treatment, and learning to manage the physical and emotional echoes left behind.
This path is intensely personal. It’s about making peace with a changed body, finding new sources of strength you never knew you had, and redefining what a full, healthy life looks like for you.
The Phases of Survivorship
Living with and beyond cancer isn't a single, static state. It’s more like a progression through different seasons, each with its own unique challenges and focus.
- Active Treatment: This is often the most intense phase, where your life can feel like it revolves around a calendar of appointments, procedures, and managing immediate side effects. The primary goal is simple: get through it.
- Post-Treatment Transition: Ringing that bell is an incredible moment, but the period that follows can be surprisingly tough. You’re moving from a highly structured, supported environment back into "normal" life, all while dealing with lingering side effects and the very real fear of recurrence.
- Extended Survivorship: This is the long game. It's about settling into a new rhythm of ongoing surveillance, managing any long-term health effects from treatment, and focusing on wellness to keep your body as strong as possible.
A Community of Strength and Hope
If you are on this path, you are in very good company. There are over 4 million women in the United States who are breast cancer survivors, making this the largest group of cancer survivors in the country. This staggering number is a testament to incredible progress in screening and treatment. In fact, the 5-year relative survival rate for all stages combined has reached an encouraging 92%.
Breast cancer survivorship is about more than just the absence of disease. It’s about quality of life, emotional wellness, and finding a way to thrive in your new reality. It's a testament to resilience and the human spirit's capacity to adapt and grow.
It's also crucial to remember that this journey looks different for everyone. Hearing from all voices enriches our understanding and strengthens the community. For instance, the experience of a Male Breast Cancer Survivor offers a vital perspective that broadens the conversation. Every story adds another layer to our collective strength, reminding us that while each path is unique, no one has to walk it alone.
Navigating Your Long-Term Medical Care
Once your active treatment wraps up, you step into a new, incredibly important phase of your health journey. This part of breast cancer survivorship is less about the intense, day-to-day fight and more about vigilant, proactive care for the long haul.
Think of it like this: treatment was the sprint, but survivorship is the marathon. It requires a different mindset—one focused on consistency, smart planning, and a deep partnership with your medical team to protect your long-term wellness.
Your follow-up care is the absolute cornerstone of this new chapter. It’s a structured plan designed to monitor your health, help you manage any lingering effects from treatment, and—most importantly—watch for any signs of cancer returning. This ongoing relationship with your care team is what keeps you in the driver's seat.
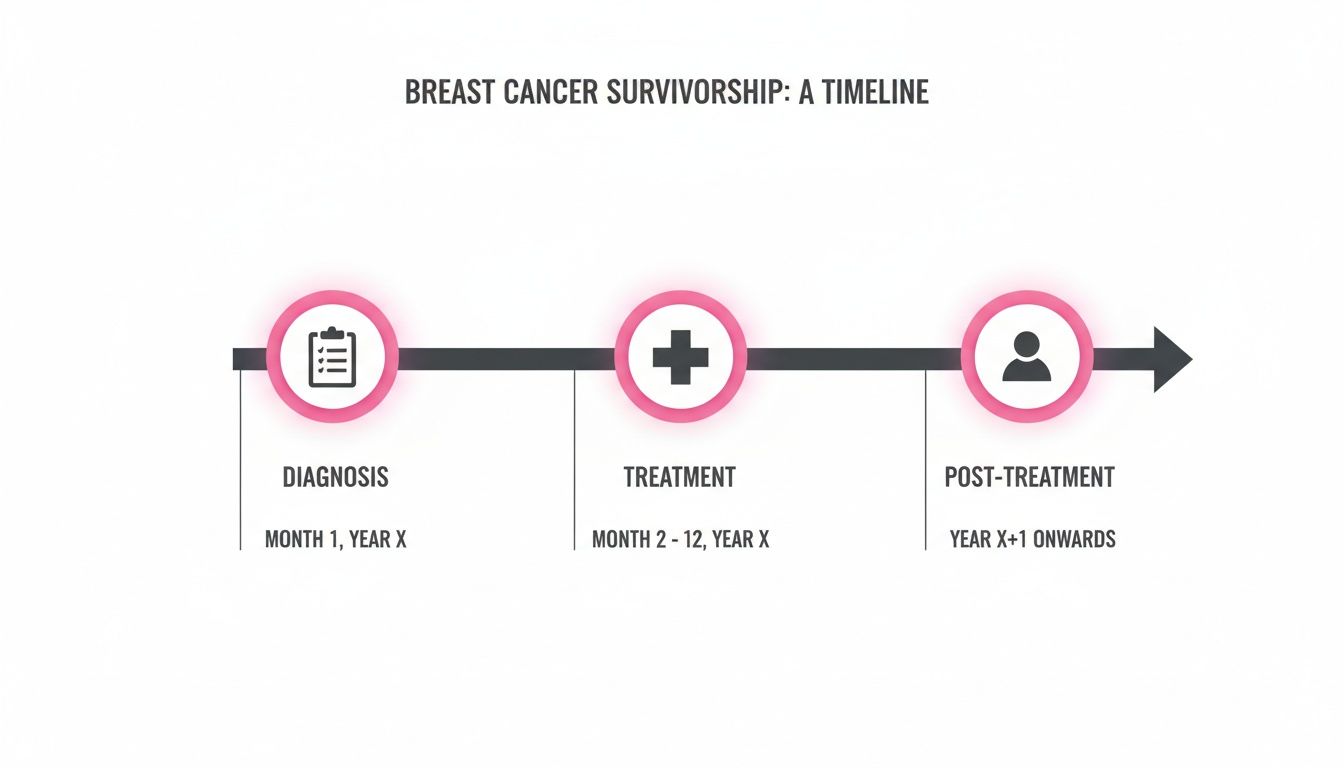
This visual helps show that survivorship isn't a single finish line. It's a continuous process that requires dedicated medical oversight long after the last treatment session ends.
Your Follow-Up Surveillance Schedule
Your oncology team will map out a personalized schedule for your follow-up visits. While the exact timing is unique to you, there’s a general rhythm to it. Right after treatment, you might see your oncologist every few months. As more time passes and you continue to do well, these visits will likely become less frequent, maybe shifting to once or twice a year.
So, what happens at these appointments? Your doctor will do a physical exam and, just as importantly, talk with you about any new symptoms or concerns. This is your time. Use it to ask every question you have. These visits are also when your team will order key surveillance tests.
Here’s a breakdown of what that typically involves:
- Mammograms: You can count on continuing with annual mammograms for any remaining breast tissue. If you had a lumpectomy, both breasts will be monitored.
- Blood Work: In some cases, specific blood tests might be used to check for signs of recurrence or to keep an eye on the long-term effects of treatments like hormone therapy.
- Other Imaging: Depending on your specific situation, your doctor might recommend other scans. For instance, bone density tests are common for women on medications known to affect bone health.
To give you a clearer picture, here is a general idea of what a follow-up schedule might look like.
Sample Follow-Up Surveillance Schedule
This table provides a general timeline for recommended medical follow-ups after completing active breast cancer treatment. Please remember, this is just a sample and your own schedule will be personalized with your oncology team.
Ultimately, this schedule is much more than just a list of appointments; it’s your safety net. It creates a regular, structured opportunity to protect your health and catch any potential issues when they are at their earliest, most treatable stage.
Managing Late and Long-Term Side Effects
Unfortunately, treatment side effects don't always vanish the day treatment ends. Some effects can linger for months or even years (these are called long-term effects), while others can pop up completely new, long after you’ve finished (known as late effects). Learning to manage these is a huge part of your survivorship care.
Some of the most common challenges survivors face include:
- Persistent Fatigue: This isn't just feeling tired. It’s a profound exhaustion that rest doesn’t seem to fix.
- Lymphedema: This is a swelling, usually in the arm, hand, or chest area on the same side as your surgery or radiation.
- Cognitive Changes: Often nicknamed "chemo brain," this can show up as frustrating issues with memory, focus, and multi-tasking.
- Neuropathy: Many people experience numbness, tingling, or pain in their hands and feet as a result of certain chemotherapy drugs.
- Bone Health Issues: Some hormone therapies, while vital for treatment, can lead to bone thinning or osteoporosis over time.
The good news? You don't just have to "live with it." Your medical team has strategies to help, from referring you to a physical therapist for lymphedema to providing nutritional counseling for fatigue. Openly discussing these issues is the first step toward improving your quality of life.
The Power of a Survivorship Care Plan
One of the most valuable tools you'll receive is a Survivorship Care Plan. Think of this document as your personal health playbook—a summary of your cancer journey and a clear roadmap for your future. It's created by your oncology team specifically for you and your primary care doctor.
A comprehensive plan will almost always include:
- A Treatment Summary: This section details your specific diagnosis, cancer stage, and a complete record of every treatment you received (surgeries, chemo drugs and doses, radiation fields, etc.).
- A Follow-Up Care Schedule: It lays out exactly which tests and appointments you need and provides a recommended timeline.
- Information on Potential Late Effects: Based on your specific treatments, this part lists possible long-term side effects and tells you which symptoms to watch for.
- Wellness Recommendations: This offers guidance on diet, exercise, and other lifestyle choices that can support your health for years to come.
This single document ensures that everyone involved in your care—from your oncologist to your family doctor—is on the same page. More than anything, it empowers you to be an active, informed advocate for your own health, making it an essential part of your life as a breast cancer survivor.
Caring For Your Emotional and Mental Health
Finishing active treatment is a huge milestone, a moment you’ve likely been waiting for. But as your body begins to heal, your mind is often just starting to process everything it's been through. This emotional recovery isn't just an afterthought; it’s a critical part of your journey that deserves just as much focus as your physical health.
It's completely normal to feel a whirlwind of conflicting emotions. One minute you might feel profound relief, and the next, a sudden wave of anxiety. The first and most important step is simply acknowledging that this complex emotional landscape is a normal part of survivorship.

Addressing Common Emotional Challenges
Many survivors discover they're navigating similar emotional territory once treatment is over. Instead of feeling like you've crossed a finish line, you might feel like you're standing in a fog, unsure of the path forward. Knowing that these feelings are common can be a powerful reminder that you are not alone.
Here are some of the hurdles you might be facing:
- Fear of Recurrence: This is, without a doubt, one of the most common fears among cancer survivors. Every new ache or twinge can send your mind spiraling into "what if" scenarios, making it tough to relax and trust your body again.
- Anxiety and Depression: The experience of a cancer diagnosis and treatment is a form of trauma. It's no surprise that many survivors grapple with lasting anxiety or depression that needs and deserves attention.
- Shifts in Body Image and Identity: Scars, hair that’s growing back differently, and other physical reminders of treatment can change how you feel in your own skin. Learning to reconnect with and feel at home in your body again is a journey of self-compassion.
- Relationship Dynamics: Cancer doesn't just happen to you; it impacts your partner, your kids, your friends. Relationships can change, and it takes patience and honest communication to navigate this new terrain. You can find more insight on this in our guide on how cancer impacts relationships.
Building Your Emotional Toolkit
You had a medical team and a treatment plan to fight the cancer. Now, it's time to build a proactive plan for your emotional well-being. This isn't about pushing down difficult feelings, but about developing resilience and finding healthy ways to cope.
Emotional recovery is an active process. It’s about intentionally creating space for your mental health, seeking out support, and giving yourself the same grace and care you’d offer a friend.
Here are a few practical tools to get you started:
- Connect with a Support Group: There's an incredible power in talking to people who just get it. Whether it’s an in-person group or an online community, sharing your story can make you feel so much less isolated.
- Practice Mindfulness and Grounding: When your mind is racing, simple techniques like deep breathing exercises, meditation, or just focusing on the sensation of your feet on the floor can pull you back to the present moment and calm the storm.
- Journal Your Thoughts: Sometimes emotions are too big or messy to say out loud. Writing them down gives you a private space to untangle your fears, frustrations, and hopes without judgment.
Knowing When to Seek Professional Help
Self-care and peer support are essential, but they aren't always enough. There is incredible strength, not weakness, in recognizing when you need the guidance of a professional. A therapist, counselor, or psychiatrist who specializes in oncology can offer targeted support.
It might be time to reach out if you notice that you're:
- Feeling overwhelmed by sadness or anxiety most days.
- Struggling to find joy in things you used to love.
- Finding that fear is holding you back from making plans for the future.
- Feeling like your emotional state is straining your relationships.
For many, the cancer journey leaves deep emotional scars. Exploring options like trauma therapy for adults can offer a structured, supportive path to process what you’ve been through. A skilled professional can equip you with coping strategies tailored to your experience, helping you move forward with a renewed sense of peace and strength.
Proactive Steps for Wellness and Recovery
After treatment ends, the focus naturally shifts. You’ve been through an intense, often grueling, fight, and now it’s time to look forward. This next phase is all about taking back the reins of your health, moving from a defensive posture against cancer to a proactive one focused on building a strong, vibrant future.
This isn't about a sudden, radical lifestyle overhaul. It’s about making smart, sustainable choices with food, movement, and specialized support that help you feel like yourself again. These are your tools for rebuilding, helping you regain control and feel empowered in your own body.

Fueling Your Body With Survivorship Nutrition
What you eat is one of the most powerful tools in your recovery toolkit. A nourishing, balanced diet can help you manage lingering side effects like fatigue, rebuild healthy tissue, and give your immune system the support it needs.
The goal isn't about strict rules or deprivation; it's about abundance and nourishment. Experts often point toward a plant-focused diet. This doesn't mean you have to become a vegetarian, but it does mean making vegetables, fruits, whole grains, and legumes the main event on your plate. Research strongly suggests this way of eating can have a real, positive impact on long-term health for survivors.
Consider these cornerstones for a survivorship-focused way of eating:
- Embrace Plant Foods: Try to fill your plate with colorful vegetables, fruits, and whole grains at every meal. They’re packed with antioxidants and anti-inflammatory compounds that your body loves.
- Choose Lean Proteins: Fish, chicken, beans, and lentils are fantastic sources of protein that help your body repair and rebuild tissue after treatment.
- Limit Processed Foods and Red Meat: It's a good idea to cut back on things like processed meats (think bacon and deli meat), sugary drinks, and foods high in saturated fats.
- Maintain a Healthy Weight: Getting to and staying at a healthy weight is one of the single most important things you can do to support your long-term health and lower future risks.
The Role of Physical Activity in Recovery
Simply put, movement is medicine. Regular physical activity is one of the best ways to fight off treatment-related fatigue, lift your mood, and improve your overall quality of life. The evidence is overwhelming: exercise is not only safe but essential for breast cancer survivorship.
Study after study shows that survivors who exercise regularly report less fatigue, sleep better, and have a much stronger sense of emotional well-being. A great target to aim for is at least 150 minutes of moderate-intensity exercise each week, but the most important step is the first one. Just start where you are.
Think of exercise not as a chore, but as a declaration of strength. Every walk, stretch, or workout is a way of reclaiming your body and actively participating in your own healing process.
Easing back into a routine after surgery or treatment needs to be done thoughtfully. Always check in with your doctor first. They’ll likely suggest starting with gentle activities like walking or stretching, then gradually building up the intensity as you feel stronger.
Leveraging Rehabilitation for a Stronger You
Sometimes, your body needs a little extra help to get back on track. Rehabilitation services aren’t a sign that something is wrong; they are a strategic part of your recovery, designed to tackle specific physical challenges and help you regain your function and confidence.
These services can make a massive difference in your day-to-day life:
- Physical Therapy (PT): A physical therapist can be your best friend for managing issues like lymphedema, post-surgery shoulder stiffness, or general weakness. They create personalized exercise plans to restore your range of motion and help you build back strength safely.
- Occupational Therapy (OT): An occupational therapist is an expert in the "occupations" of daily life. If fatigue or cognitive fog ("chemo brain") makes everyday tasks like cooking or getting work done feel overwhelming, an OT can teach you practical strategies and energy-saving techniques to manage better.
- Lymphedema Therapy: If you notice swelling (lymphedema), a certified lymphedema therapist offers specialized care, including gentle massage, compression garments, and specific exercises to get the condition under control.
Figuring out the physical recovery after surgery can feel like a journey in itself. For a more detailed look at what to expect and how to prepare, you can learn more about life after breast cancer surgery in our guide. We want to give you the resources you need to build a stronger, healthier future, one step at a time.
Understanding and Managing Recurrence Fears
The fear of cancer coming back is one of the toughest, most persistent parts of being a breast cancer survivor. It’s completely normal. Years after treatment, a new ache or an unfamiliar pain can still send a jolt of anxiety through you, making it hard to feel like you’ve truly moved on. This fear is real, valid, and something nearly every survivor grapples with.
But you don't have to let that anxiety run your life. The best way to regain control is to arm yourself with good, clear information. When you understand what recurrence actually means—and just as importantly, what it doesn't—you can shift from a state of constant worry to one of watchful awareness. It empowers you to become a proactive partner with your healthcare team, focusing on what you can actually control.
Distinguishing Between Types of Recurrence
When your oncologist talks about recurrence, they simply mean the cancer has returned after a period where it was undetectable. It’s crucial to know that not all recurrences are the same. The type of recurrence has a massive impact on your prognosis and treatment plan.
There are three main categories:
- Local Recurrence: The cancer has reappeared right where it started—in the same breast or in the scar tissue on the chest wall after a mastectomy.
- Regional Recurrence: This is when the cancer shows up in the lymph nodes close to the original tumor, like those under the arm or near the collarbone.
- Distant Recurrence (Metastasis): This is the one people fear most. It means cancer cells have traveled to other parts of the body. The most common sites are the bones, liver, lungs, or brain.
Just knowing these differences can help manage the fear. A local or regional recurrence is serious, of course, but it can often be treated effectively, with the goal of another cure.
Knowing the Signs Without Being Overwhelmed
Being vigilant doesn't mean living in a constant state of high alert. It's about getting to know your "new normal" and recognizing what kinds of changes are worth a call to your doctor. Aches and pains are a part of life, but some symptoms are more specific.
Your goal is not to become a self-diagnostician, but to be an informed observer of your own body. This allows you to report changes to your medical team promptly and confidently, without panicking over every minor symptom.
Pay attention to any new symptoms that don't go away, such as:
- A new lump, thickening, or firmness in your breast, chest wall, or armpit.
- Changes to the skin on your breast, like puckering, redness, or swelling.
- Any new nipple discharge, a nipple that turns inward, or a persistent rash.
- Pain in one specific spot—like your chest or bones—that is persistent and doesn't get better.
- Unexplained weight loss, a nagging cough, or shortness of breath.
- Headaches or vision changes that stick around.
Seeing one of these signs isn't a reason to assume the worst, but it is a reason to make an appointment. We cover this in much more detail in our guide on the signs of breast cancer recurrence.
A Modern View of Advanced Disease
For some survivors, the journey involves learning to live with distant, or metastatic, disease. While that diagnosis is undoubtedly serious, how we approach it has changed dramatically. With breakthroughs in targeted therapies, immunotherapies, and even gentler chemotherapies, many people now manage metastatic breast cancer as a chronic condition.
The goal shifts from a one-time cure to long-term control. The focus is on maintaining a high quality of life for as long as possible. This approach allows people to live for many years, managing their illness with treatments that are effective but have fewer life-disrupting side effects. It’s a powerful testament to how far cancer care has come, offering a real path forward and sustained hope.
Finding Your Advanced Survivorship Care Team in New York
The last piece of the puzzle—and honestly, the most critical one—is finding the right medical team to walk with you for the long haul. When you're dealing with a complex diagnosis or living with advanced breast cancer, this means looking for a practice that goes far beyond the standard playbook.
You need a partner in your care. Someone who sees the whole you, not just a chart full of data.
For those in Brooklyn, New York, Hirschfeld Oncology embodies this very personal, patient-focused approach to survivorship. The practice is led by Dr. Azriel Hirschfeld, a physician with over two decades of experience dedicated to creating real, tangible hope for people who need it most—especially those who may feel like they're running out of road.
A Different Way of Thinking About Treatment
At Hirschfeld Oncology, the core philosophy is simple but powerful: manage the disease effectively while protecting, and even enhancing, your quality of life. This isn't just a vague promise; it's a commitment carried out through carefully personalized strategies that aim to lessen the harsh side effects that can make everyday life feel like a battle.
It’s all about finding that perfect balance for you.
Key treatment approaches you’ll find here include:
- Low-Dose Chemotherapy: Think of this as a gentler, more sustainable way to keep cancer in check. By using smaller, more frequent doses, it minimizes toxicity and helps you feel more like yourself day-to-day.
- Targeted Therapies: These are smarter, more precise treatments. Instead of a widespread attack, they zero in on specific features of the cancer cells, which often means fewer side effects and a better outcome.
This thoughtful strategy means your care plan is truly built around your life and your goals. You're not just a passenger; you're in the driver's seat.
True survivorship care isn't just about fighting cancer. It's about charting a sustainable path forward that allows you to live, and live well. It's a team effort built on hope, resilience, and taking back your future.
If you live in Williamsburg, Bushwick, or anywhere in the greater NYC area, taking the next step is simple. You can schedule a consultation at Hirschfeld Oncology to see what a higher standard of survivorship care feels like. It’s an opportunity to find a compassionate team that is ready to explore every possible path forward, right alongside you.
Answering Your Questions About Life After Treatment
It’s completely normal to have a lot of questions as you move into the next phase after breast cancer treatment. Let's walk through some of the most common ones that come up, so you can feel more confident about the road ahead.
What Is a Survivorship Care Plan and Why Is It So Important?
Think of a survivorship care plan as your personalized health roadmap for life after treatment. It’s a detailed document that pulls everything together: your specific diagnosis, a summary of all the treatments you went through, and a clear schedule for your future medical care. It maps out all your follow-up appointments, surveillance tests, and critical information on potential long-term side effects to watch for.
This plan is incredibly valuable. It acts as a bridge, ensuring your oncology team and your primary care doctor are on the same page about your health history and future needs. Most importantly, it empowers you. It gives you the information you need to be an active, informed partner in your own health care, not just a passive patient.
How Do I Deal With the Fear of My Cancer Coming Back?
The fear of recurrence is one of the most common and challenging parts of survivorship. It's a heavy weight to carry, but the key is not letting that anxiety take over your life. A powerful first step is to focus on what you can actually control. That means diligently keeping up with your follow-up appointments and making positive lifestyle choices, like eating well and staying active.
It's also crucial to find healthy ways to process your anxiety. Many people find immense relief in support groups, where you can connect with others who truly get what you’re going through. You might also explore mindfulness, journaling, or talking with a therapist who specializes in working with cancer survivors. These are all excellent tools for learning to manage those persistent fears.
"When does someone become a survivor? The consensus is that survivorship begins at diagnosis and continues for the rest of a person's life. It is not an end point, but a continuous journey."
This shift in perspective is so important. It recognizes that your entire experience—from the moment you were diagnosed—is part of your survivorship story.
Is There Anything I Can Do to Lower My Risk of Recurrence?
Yes, absolutely. While nothing can offer a 100% guarantee, there are meaningful, proactive steps you can take to support your long-term health and potentially lower your risk. One of the most significant factors you can influence is maintaining a healthy body weight.
Beyond that, research points to several other powerful actions:
- Get moving regularly: Aim for at least 150 minutes of moderate-intensity exercise, like a brisk walk or bike ride, every week.
- Focus on a balanced diet: Build your meals around vegetables, fruits, and whole grains. It’s also wise to limit alcohol, highly processed foods, and red meat.
- Stick with your long-term therapies: If your doctor prescribed ongoing medication like hormone therapy, taking it exactly as directed is a critical piece of your risk-reduction strategy.
When Am I Officially Considered a "Survivor"?
From the very day you were diagnosed. The medical community views breast cancer survivorship as a journey that starts at diagnosis and continues for the rest of your life. This definition is meant to be inclusive, honoring every single part of the experience—the difficult treatments, the recovery, and the new reality of living beyond cancer. While the term is a personal one, know that you've been a part of this community from day one.
At Hirschfeld Oncology, we know survivorship is an ongoing journey that deserves dedicated, compassionate support. We specialize in creating personalized, long-term care plans to help you thrive for years to come. You can learn more about our approach and find helpful resources on our blog.





.png)


.png)
.png)




