Hearing the words "triple-negative breast cancer" can be unnerving, partly because the name itself sounds so clinical and confusing. It’s a diagnosis defined not by what the cancer cells have, but by what they lack.
This specific type of breast cancer tests negative for three common receptors—estrogen, progesterone, and HER2—which act like fuel for many other breast cancers. Since these receptors aren't present, the standard hormonal therapies that target them won't be effective, which means we need to take a different, more direct approach to treatment.
What a Triple Negative Breast Cancer Diagnosis Means
When you're first diagnosed, it's easy to get lost in the terminology. Let's break it down with a simple analogy. Think of a cancer cell as a small house with locks on the door. Most breast cancer treatments are like highly specific keys designed to fit those locks (the receptors) and shut down the house's power, stopping the cancer's growth.
With triple-negative breast cancer (TNBC), the cancer cells are missing the three most common locks:
- Estrogen Receptors (ER-negative): These cells don't have the "lock" that the hormone estrogen can open, so they don't depend on it to grow.
- Progesterone Receptors (PR-negative): In the same way, they lack the receptors for progesterone, another hormone that can fuel cancer growth.
- HER2 Receptors (HER2-negative): They also don't have an overabundance of the HER2 protein, a powerful growth signal in other types of breast cancer.
Because TNBC cells are missing these specific targets, treatments designed to block them—like tamoxifen or Herceptin—simply have nothing to latch onto. It's like trying to use a key on a door with no lock. This is the fundamental reason why the treatment journey for TNBC is so different.
To give you a clearer picture, this table breaks down what each "negative" status means.
Understanding Your Cancer's 'Negative' Status
Essentially, your pathology report is telling us which "keys" we can't use, which helps us focus on the ones that will work.
Why This Biology Matters for Treatment
The "triple-negative" status has historically made chemotherapy the go-to treatment. Chemo works by attacking all cells that divide quickly, and since many TNBC tumors grow rapidly, it can be quite effective.
But the good news is that we've moved far beyond relying on chemo alone. The treatment landscape has evolved significantly, and we now have more sophisticated tools like immunotherapy, PARP inhibitors, and antibody-drug conjugates that can be used alongside chemotherapy to fight this cancer more intelligently.
Understanding the unique biology of your tumor is the first step toward empowerment. It transforms a complex diagnosis into a clear reason for your personalized treatment plan, helping you and your care team navigate the path forward with confidence.
Triple-negative breast cancer is a distinct and often aggressive subtype, making up about 15-20% of all breast cancers diagnosed. In the United States, that translated to an estimated 45,000 new cases in 2023, with that number expected to climb. If you're interested in the data, you can explore the market report from DelveInsight. These numbers highlight just how critical it is to continue advancing research and providing specialized, expert care for every person facing this diagnosis.
The Diagnostic Journey: From Biopsy to Staging
It all starts with a suspicious mammogram or a lump you can feel. That initial discovery kicks off a diagnostic journey—a series of carefully coordinated steps designed to give us a complete picture of what's going on. Think of it as detective work. Each test provides another crucial clue, helping us understand the cancer's identity, its characteristics, and how far it has spread.
The first and most definitive step is the biopsy. In this procedure, a small piece of tissue is taken from the suspicious area and sent to a pathologist. This is the specialist who looks at the cells under a microscope to answer the most fundamental question: is it cancer? If the answer is yes, their work has just begun.
Confirming Triple-Negative Status
For breast cancer, the pathologist's next job is to figure out its specific subtype. To confirm a triple-negative breast cancer (TNBC) diagnosis, they test the cancer cells for three specific receptors: estrogen (ER), progesterone (PR), and a protein called HER2.
As we covered earlier, TNBC gets its name because it lacks all three. The cells are "negative" for all of them. This is a critical piece of information because it immediately tells your oncology team that standard treatments like hormone therapy or HER2-targeted drugs won't work. We have to find a different way to attack the cancer.
This simple flowchart illustrates the logic perfectly.
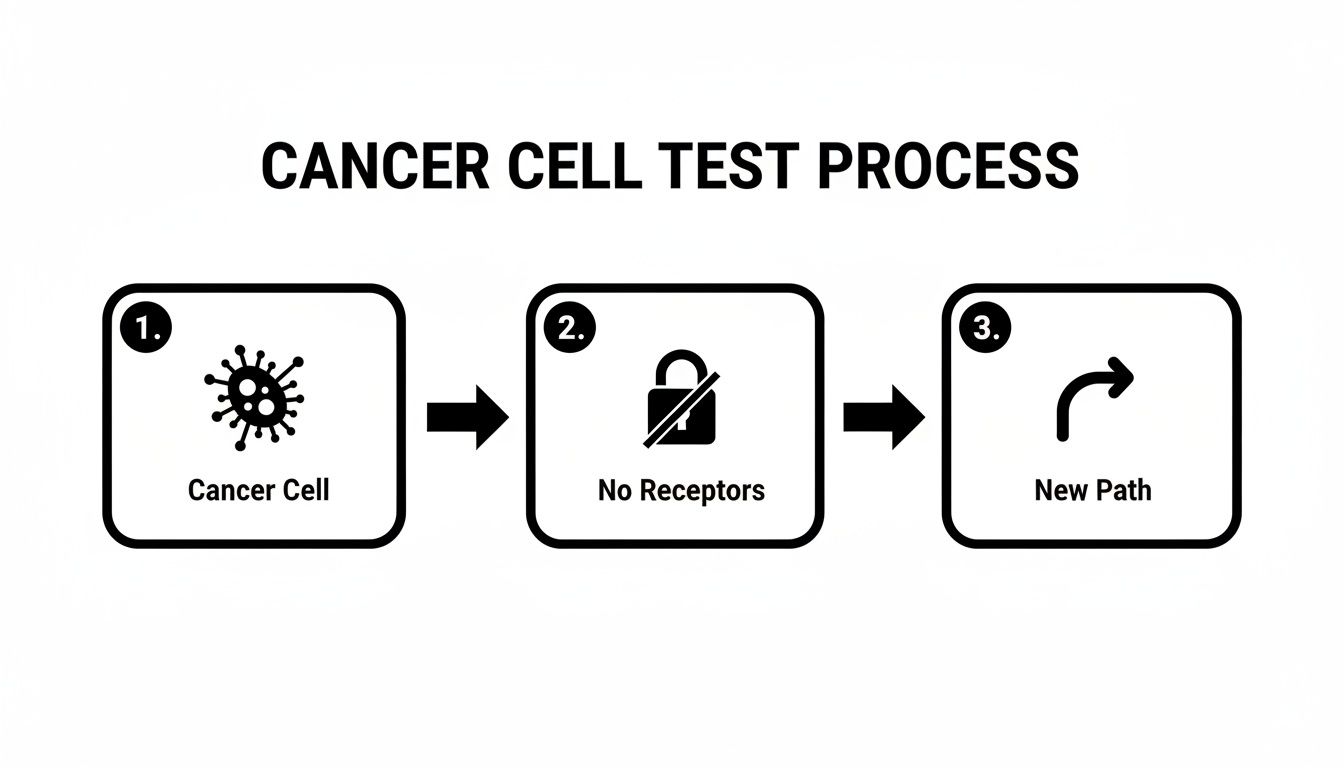
When the usual "locks" aren't there for our therapeutic "keys" to fit into, we have to forge a new path. That means looking for the cancer's other vulnerabilities.
Looking Deeper with Biomarker and Genetic Testing
Beyond just the ER, PR, and HER2 status, we need to create a more detailed molecular portrait of the tumor. For TNBC, two other tests have become absolutely vital:
- PD-L1 Testing: This test measures a protein called Programmed Death-Ligand 1 on the surface of the cancer cells. High levels of PD-L1 can act like a "don't see me" cloak, hiding the cancer from your immune system. If your tumor has high PD-L1 levels, it's often a great candidate for immunotherapy drugs that unmask the cancer cells, allowing your own immune system to attack them.
- BRCA Gene Mutation Testing: A significant portion of TNBC cases are driven by inherited mutations in the BRCA1 or BRCA2 genes. We strongly recommend genetic testing for these mutations. If you test positive, it opens the door to highly effective targeted therapies called PARP inhibitors, which are designed specifically to exploit this genetic weakness in the cancer cells.
Getting the full results from your pathology report is incredibly empowering. We know the medical language can be intimidating, so we've put together a guide to help you make sense of it all. You can learn more about how to read a pathology report on our blog.
Determining the Cancer's Stage
Once we’ve confirmed the diagnosis and understand its molecular drivers, the next step is staging. Staging is all about figuring out the extent of the cancer—how big the tumor is and if, or where, it has spread. This usually involves imaging tests like CT scans, PET scans, or an MRI.
We use the universal TNM system to classify the stage:
- T (Tumor): How large is the primary tumor?
- N (Node): Has the cancer spread into nearby lymph nodes?
- M (Metastasis): Has the cancer spread to distant parts of the body, like the lungs, liver, or bones?
The T, N, and M values are combined to determine an overall stage, from Stage I (very early and localized) to Stage IV (metastatic). Knowing the precise stage is fundamental, as it dictates the entire goal of treatment—whether we're aiming for a cure or focusing on long-term management and quality of life.
How Modern Medicine Fights Triple Negative Breast Cancer

The approach to treating triple-negative breast cancer (TNBC) has come a long way from a one-size-fits-all strategy. Today, our focus is on building a personalized regimen that attacks the cancer from multiple angles, always balancing aggressive treatment with your quality of life. The goal is a plan as unique as your tumor's own biology.
This means we've shifted from broad-spectrum attacks to much smarter, more focused assaults on cancer cells. Let’s walk through the powerful tools we now use to fight this complex disease.
The Cornerstone Of Treatment: Chemotherapy
For years, chemotherapy has been the main weapon against TNBC. Because these cancer cells grow and divide so quickly, they are especially susceptible to chemotherapy drugs, which are designed to kill rapidly growing cells.
While effective, this widespread approach can also damage healthy cells, which is what causes many of the challenging side effects. Still, it remains a critical part of treatment for both early-stage and advanced TNBC, often used to shrink tumors before surgery or to clear out any cancer cells left behind. You can learn more in our detailed guide on the role of chemotherapy in breast cancer treatment.
Modern oncology is all about using chemo more strategically. We often pair it with newer treatments that boost its effectiveness or allow us to use lower, less toxic doses. It’s no longer the only option, but a foundational part of a much larger, more sophisticated plan.
Unleashing The Immune System With Immunotherapy
One of the biggest breakthroughs in recent years has been immunotherapy. Think of your immune system as a 24/7 security patrol, always on the lookout for threats. Cancer cells can be devious, though. They sometimes figure out how to wear a disguise, tricking the immune system into leaving them alone.
A key part of this disguise is a protein called PD-L1. When a cancer cell is covered in PD-L1, it’s like it’s holding up a "friendly" sign to an immune cell, telling it not to attack.
Immunotherapy drugs called checkpoint inhibitors, like pembrolizumab (Keytruda®), are designed to block this signal. They essentially rip the disguise off the cancer cells, finally allowing your own immune system to recognize them as a threat and destroy them.
For patients whose TNBC tumors express this PD-L1 protein, combining immunotherapy with chemotherapy is now a standard of care. This approach empowers your own body to join the fight, often leading to longer-lasting results.
Exploiting Genetic Weaknesses With PARP Inhibitors
Some TNBC cases are tied to an inherited genetic mutation, most often in the BRCA1 or BRCA2 genes. These genes are supposed to be the body's DNA repair crew, fixing damage to keep cells healthy and stable.
When someone has a BRCA mutation, that repair crew is short-staffed. The cancer cells with this mutation are working with a major vulnerability; they’re already struggling to fix their own DNA.
PARP inhibitors, like olaparib (Lynparza®) and talazoparib (Talzenna®), are a class of drugs that exploit this very weakness. They work by knocking out a backup DNA repair pathway that these fragile cancer cells depend on. Without their primary or backup repair kits, the cancer cells accumulate so much DNA damage that they simply self-destruct, leaving most healthy cells alone.
This is a brilliant example of personalized medicine—turning a specific genetic vulnerability into a precise, effective target.
Delivering Treatment Like A Guided Missile: ADCs
Another incredibly powerful strategy uses what are known as antibody-drug conjugates (ADCs), often called "smart chemo." You can think of these drugs as guided missiles designed to deliver a toxic chemotherapy payload directly to cancer cells, sparing healthy tissue along the way.
An ADC has two key parts:
- An Antibody: This part is like a heat-seeking system, engineered to find and lock onto a specific protein (or target) found on the surface of cancer cells. For TNBC, a major target is a protein called Trop-2.
- A Drug Payload: This is a potent chemotherapy drug that is attached to the antibody.
The ADC travels through your bloodstream until the antibody finds its target on a cancer cell. Once it latches on, the cancer cell pulls the ADC inside, and the toxic payload is released, killing the cell from within.
Sacituzumab govitecan (Trodelvy®) is a groundbreaking ADC that targets Trop-2 in TNBC. It provides a vital and effective option for patients whose cancer has returned or progressed. This approach lets us maximize the cancer-killing power while minimizing the collateral damage.
A Snapshot Of Modern TNBC Treatment Options
Navigating these therapies can be complex. The table below breaks down the main treatment types to give you a clearer picture of how each one works and who it's designed to help.
Each of these approaches represents a significant step forward, giving us more ways to tailor treatment directly to the unique features of your cancer.
Managing Your Well-Being Through Treatment

Getting through treatment for triple-negative breast cancer isn’t just about the medicine. It’s about taking care of you—your whole self—to stay strong and maintain your quality of life along the way. The treatments used to fight TNBC are powerful, and they often come with significant side effects that need their own management plan.
This is where supportive care comes in. Think of it as a crucial part of your overall strategy. By getting ahead of potential side effects, you and your care team can work together to keep you feeling as good as possible. Your voice is the most important tool here, so never hesitate to speak up about any new or worsening symptoms.
Addressing Common Chemotherapy Side Effects
Chemotherapy remains a cornerstone of TNBC treatment, but it can be tough on the body. The most common challenges patients face are nausea, vomiting, deep fatigue, and hair loss. Thankfully, we have excellent ways to manage them.
- Nausea and Vomiting: Today’s anti-nausea medications are incredibly effective. Your oncologist will likely have you start taking them before your infusion even begins, a preemptive strike to stop nausea in its tracks.
- Fatigue: This isn't just everyday tiredness; it’s a profound sense of exhaustion. It might sound counterintuitive, but gentle movement like a short walk can actually boost your energy. Prioritizing rest and good nutrition is also non-negotiable.
- Hair Loss: While this is often one of the most emotionally difficult side effects, hair loss from chemo is almost always temporary. Some patients find success with cold capping, a therapy used during infusions to help reduce hair loss by constricting blood vessels in the scalp.
Proactive management is your best defense. Instead of waiting for a side effect to become severe, tell your medical team as soon as it begins. Early intervention can make a world of difference in your comfort and ability to stay on schedule with your treatment.
Food is your fuel, and getting the right nutrition can make a huge impact. To learn more, take a look at our practical guide on what to eat during chemotherapy.
Managing Unique Reactions to Newer Therapies
As TNBC treatments advance, we see new types of side effects. Immunotherapy and PARP inhibitors, for instance, have their own distinct profiles that are very different from traditional chemotherapy.
Immunotherapy works by unleashing your immune system to fight the cancer. Sometimes, though, an over-activated immune system can mistakenly attack healthy tissues, causing inflammation. This might show up as a skin rash, diarrhea (colitis), or problems with hormone-producing glands like the thyroid. It’s absolutely critical to report these symptoms right away, as they often require specific medical intervention.
PARP inhibitors can lower your blood counts, which might lead to anemia (low red blood cells) and fatigue. This is why regular blood tests are part of the routine—they allow us to catch these changes early and manage them, often with a simple dose adjustment or other supportive medications.
The Role of Integrative and Supportive Care
A truly comprehensive plan weaves medical treatment together with therapies that support your whole person. These integrative strategies don't treat the cancer directly, but they can dramatically improve how you feel throughout your journey.
Many of our patients find real relief and a better quality of life by incorporating practices like:
- Acupuncture: Often used to help control treatment-related nausea and pain.
- Gentle Exercise: Activities like yoga or walking are fantastic for fighting fatigue and lifting your mood.
- Mindfulness and Meditation: These are powerful tools for managing the natural stress and anxiety that come with a cancer diagnosis.
It’s important to talk with your oncologist before starting any new complementary therapy to make sure it's a safe and appropriate choice for you. By combining cutting-edge medicine with thoughtful, holistic support, you can protect your strength and well-being, empowering you to face your treatment with greater comfort and resilience.
Finding the Right Partner in Your Cancer Care
A diagnosis like triple-negative breast cancer is complicated, and the journey requires more than just medicine. It demands a true partnership. Choosing your oncology team is probably one of the most important decisions you'll make, because this relationship is the anchor for everything that follows.
The right team doesn’t just see a diagnosis; they see you. They treat the cancer, of course, but they also treat you as a whole person, taking the time to understand your goals and protect your quality of life at every turn.
That philosophy is the bedrock of everything we do at Hirschfeld Oncology. We believe real partnership means building a treatment plan together—one that is as unique as you are. It's a conversation, a collaboration where your voice is not just heard but is essential to the process.
What Personalized Care Actually Looks Like
A personalized care plan isn't about simply following a standard flowchart. It's about finding the most effective path forward for you, one that is also the least toxic. For TNBC that has spread or is resistant to initial treatments, this often means getting creative with strategies designed to outsmart the cancer while preserving your strength.
What might this involve?
- Low-Dose Chemotherapy: Sometimes, smaller, more frequent doses of chemotherapy can keep the cancer in check just as effectively but with far fewer of the harsh side effects that can diminish your quality of life.
- Intelligent Drug Combinations: We might pair a targeted therapy or an immunotherapy agent with chemotherapy. The idea is to create a combined attack that's more powerful than any one of those drugs could be on its own.
- Access to Clinical Trials: For some people, the best and most promising options aren't yet standard of care. They're found in clinical trials testing the next generation of cancer therapies.
The goal is always to strike the right balance: fighting the disease aggressively while fiercely protecting your quality of life. It’s not an either/or choice. It’s about achieving both with a thoughtful, customized strategy.
A Research-Driven Approach in New York City
Here at Hirschfeld Oncology, we bring this approach to life for our patients in the New York City area. Our care is compassionate, but it’s also driven by the latest research. We know that hope comes from having options, especially when standard treatments haven't worked or have stopped working. Our focus is on crafting plans that directly target the unique biology of your tumor.
We are committed to giving you the knowledge and control you need to be an active participant in your own care. Every meeting is a conversation. We explain the "why" behind every recommendation, talk openly about the potential side effects and benefits, and make sure the plan aligns with what truly matters to you.
You are never just a patient here—you are the central member of your own care team. This collaborative spirit ensures your treatment plan isn't just medically sound, but that it also fits your life and your goals. When you partner with a team that truly values your input, you can face your breast cancer triple negative journey with more confidence and a real sense of hope.
Thriving After Triple Negative Breast Cancer Treatment
Finishing your main course of treatment for triple-negative breast cancer is a huge moment. It’s a turning point, shifting from the intensity of active therapy to a new chapter focused on recovery, long-term health, and careful monitoring. We often call this phase “survivorship.”
Your partnership with our oncology team doesn't end here. Instead, it changes. The focus now is on helping you thrive for years to come.
What Your Follow-Up Care Involves
After you've completed treatment for early-stage triple-negative breast cancer, we'll see you regularly. A typical schedule might look like a visit every few months for the first two to three years, then gradually less often after that.
Why so often at first? The risk of TNBC coming back is highest in these initial years, so keeping a close eye on things is our top priority.
During these appointments, we’ll do a physical exam and, most importantly, talk about how you're feeling and any new concerns you might have. Regular mammograms on any remaining breast tissue (and the other breast) are also a standard part of your long-term plan. Other scans, like CT or PET scans, aren’t usually done routinely unless you develop specific symptoms that we need to investigate.
Think of your follow-up plan as your health roadmap for the future. It’s designed to give you peace of mind and ensure that if any issues do come up, we catch and address them as early as possible.
Creating Your Survivorship Care Plan
A survivorship care plan is an incredibly useful document that pulls together your entire cancer journey and maps out a clear path for your future health. It's something we create together.
It usually includes:
- A Treatment Summary: This is a detailed record of your diagnosis, the exact treatments you had (chemotherapy, immunotherapy, surgery, radiation), and the dates you received them.
- A Follow-Up Schedule: A simple timeline showing when you need to come in for appointments, blood work, and imaging scans.
- Managing Long-Term Effects: Practical guidance for handling potential lingering side effects from treatment, like fatigue, neuropathy (nerve pain), or what some people call "chemo brain."
- Wellness Recommendations: Real-world advice on lifestyle choices that can support your health and may help lower the risk of the cancer returning.
This plan puts all the information in your hands, empowering you to take an active role in your health. It’s also a fantastic communication tool for your other doctors, like your primary care physician, to make sure everyone is on the same page.
Finally, survivorship is about reclaiming your sense of well-being. Simple, healthy choices make a big difference. Regular physical activity—aiming for about 150 minutes of moderate exercise a week—can do wonders for fatigue and your quality of life. A balanced diet and finding ways to manage stress are also powerful tools in your long-term wellness strategy, helping you feel strong, healthy, and back in control.
Your Questions About TNBC, Answered
When you're first diagnosed with triple-negative breast cancer (TNBC), it’s completely normal to feel overwhelmed and have a million questions running through your mind. Getting clear, honest answers is one of the best ways to feel more grounded and in control. Let's walk through some of the most common questions we hear from patients and their families every day.
Why Do Doctors Call Triple-Negative Breast Cancer "Aggressive"?
You’ll often hear TNBC described as "aggressive," which can be a scary word. This term really comes down to two key factors. First, the cancer cells themselves tend to grow and multiply faster than in other common types of breast cancer. Because of this rapid growth, it's sometimes discovered at a later stage.
Second, the "triple-negative" name tells us what it lacks: the three most common receptors—estrogen, progesterone, and HER2. These receptors act like docking stations that many of today's most effective breast cancer drugs target. Without them, standard hormonal therapies and HER2-targeted drugs simply won't work, which often means we need to turn to more intensive treatments like chemotherapy. TNBC also has a higher statistical risk of coming back in the first few years after treatment compared to hormone-positive cancers.
Is Genetic Testing Really Necessary for TNBC?
Yes, without a doubt. We consider genetic testing, especially for inherited mutations in the BRCA1 and BRCA2 genes, to be a standard and essential part of the workup for every single patient with TNBC. This is because a significant portion of triple-negative cases are directly tied to an inherited BRCA1 mutation.
Finding out your genetic status isn't just a piece of trivia—it can completely change your treatment options.
- Unlocks Targeted Treatments: If a BRCA mutation is found, you may become a candidate for a class of drugs called PARP inhibitors. These smart drugs are specifically designed to exploit a weakness that exists only in cancer cells with that particular genetic flaw.
- Empowers Your Family: This information is also a powerful gift to your family members. It gives them the knowledge they need to make informed decisions about their own cancer screening and prevention strategies.
Can My Diet Actually Make a Difference?
While there's no diet that can cure cancer, what you eat and how you live absolutely play a crucial supportive role. Think of good nutrition as a way to fortify your body for the fight ahead. A well-balanced diet rich in nutrients helps you maintain strength, cope better with treatment side effects like fatigue, and support your immune system's recovery.
Gentle movement, as cleared by your doctor, is another powerful tool. Studies have consistently shown that light exercise can dramatically reduce fatigue and lift your spirits. Taking charge of your nutrition and staying active are tangible ways you can partner in your own care, improving your quality of life and sense of well-being.
What Should I Ask My Oncologist About TNBC?
Walking into your oncologist's office with a list of questions is one of the most empowering things you can do. You are the most important member of your care team, and being prepared helps ensure you understand your diagnosis and feel confident in the plan.
It’s important to ask direct questions to get the clarity you need. There is no such thing as a "bad" question when it comes to your health.
Here are a few essential questions to get the conversation started:
- Can you explain the specific stage and grade of my cancer?
- Have biomarker tests, like PD-L1, been performed on my tumor tissue?
- Do you recommend I undergo genetic testing for BRCA mutations?
- What are all of my possible treatment options, including any clinical trials I might be eligible for?
- What side effects should I expect from the recommended treatment, and how can we manage them from the start?
At Hirschfeld Oncology, we believe answering your questions is the first step in building a strong, trusting partnership. If you're looking for a second opinion or a personalized care plan focused on both effectiveness and your quality of life, we invite you to connect with our team. You can learn more about our unique approach and find patient resources at https://honcology.com/blog.





.png)


.png)
.png)




