When you hear "chemotherapy," it's natural for your mind to jump to side effects. The most common ones with carboplatin are things like fatigue, nausea, and a temporary dip in your blood cell counts. But here’s the important part: while we expect these reactions, modern oncology has gotten incredibly good at managing them.
Many patients find the treatment much more tolerable than they first imagined.
Understanding Your Carboplatin Treatment Journey

Starting carboplatin often comes with a mix of hope and nervousness. It's a powerful and effective tool in our arsenal against cancers of the ovary, lung, head, and neck, among others. Carboplatin is part of a family of drugs called platinum-based agents, which are designed to damage the DNA inside cancer cells, stopping them from making copies of themselves.
Think of it like this: cancer cells grow by dividing relentlessly. Carboplatin throws a wrench into that machinery by scrambling their genetic instructions. When a cell can't replicate its DNA properly, it can't divide, and the cancer's growth is halted.
Setting Realistic Expectations for Side Effects
So, what about the side effects? The main reason they happen is that carboplatin, while targeting fast-growing cancer cells, can sometimes affect other healthy cells that also divide quickly. This includes cells in your bone marrow (which make blood), hair follicles, and the lining of your mouth and digestive tract.
But "common" doesn't mean "unavoidable" or "severe." After decades of using this medication, we’ve developed a solid playbook for anticipating, preventing, and treating these effects. Your care is about more than just fighting the cancer; it's about keeping you strong and comfortable through the process.
This patient-first approach means we're always a step ahead.
- Proactive Medications: We don't wait for nausea to start. You’ll get powerful anti-nausea medications right before your infusion to head it off.
- Close Monitoring: Regular blood tests are our window into what’s happening inside. They let us track your blood counts closely and adjust your treatment schedule to give your body time to recover.
- Personalized Strategies: No two patients are the same. Your overall health, specific cancer, and other treatments you might be receiving all shape your unique supportive care plan.
Your oncology team is prepared for these side effects. Open communication about how you're feeling is the key to ensuring your comfort and safety throughout the treatment process. Our guide on what to expect from chemotherapy offers more general insights into this journey.
A Quick Look at Common Side Effects
To help you get a clearer picture, it’s helpful to see the most frequent side effects in one place. Just remember, everyone's experience is different—you might have a few of these, or none at all. The intensity varies widely, too.
Here is a simple breakdown of what many patients can expect.
Common Carboplatin Side Effects At a Glance
This table gives you a roadmap, but your care team will provide the detailed guidance you need to navigate any of these issues if they arise.
Managing Common Carboplatin Side Effects

To really get a handle on managing side effects, it helps to first understand why they happen. I often tell my patients to think of their body as a carefully tended garden. Carboplatin is a highly effective weed killer, designed to go after the fastest-growing things in that garden—the cancer cells. But sometimes, it can't quite tell the difference between a weed and other healthy, fast-growing "plants," like the cells in your bone marrow, stomach lining, or hair follicles.
So when you start to feel certain effects, it's not a sign that something has gone wrong. On the contrary, it's evidence that the treatment is doing its job throughout your body. The best part is that these reactions are temporary, we know how to anticipate them, and we have a whole playbook of strategies to keep you comfortable.
Conquering Nausea and Digestive Discomfort
The thought of nausea is often what worries patients most, but this is an area where oncology care has made incredible progress. We don't just wait for you to feel sick; we get ahead of it. Before your infusion even starts, we’ll give you powerful anti-nausea medications (known as antiemetics) to head off those signals in your brain before they can cause trouble.
Historically, gastrointestinal issues were a major challenge, affecting over 90% of patients in early clinical trials. Thankfully, the antiemetic drugs we use today have completely changed that experience for the better.
Your care team will also send you home with a clear, personalized plan that usually includes:
- Round-the-Clock Meds: A prescription to take on a set schedule for a few days post-infusion, even if you feel perfectly fine. This prevents nausea from ever getting a foothold.
- "As-Needed" Backups: An extra medication you can take if any breakthrough queasiness sneaks through.
- Smart Food Choices: Simple advice like eating smaller, more frequent meals and steering clear of greasy or heavily spiced foods can make a world of difference.
Finding what works for you is key. Our guide on cancer-related nausea has even more practical tips you can try.
Overcoming Pervasive Fatigue
Chemo fatigue isn't your average, end-of-a-long-week tiredness. It’s a profound, bone-deep exhaustion that sleep doesn't always seem to fix. This happens because your body is working overtime, using a massive amount of energy to process the medication and repair healthy cells that were caught in the crossfire.
While it's one of the most common carboplatin side effects, you don't have to just accept it. The secret is to learn to work with your body instead of fighting against it.
Patient Tip: Think of your daily energy like a phone battery. You start each day with a certain charge. Be intentional about how you spend it. Prioritize what matters most, and don't hesitate to delegate or ask for help with the rest. Conserving your energy is a strategy, not a weakness.
A few small lifestyle shifts can have a surprisingly big impact on your energy levels:
- Gentle Movement: It sounds counterintuitive, but a short, slow walk can actually boost your energy more than staying on the couch.
- Power Naps: If you need to nap, keep it brief—around 20 to 30 minutes. This will give you a refresh without messing up your nighttime sleep.
- Hydration is Key: Dehydration is a huge energy drain. Make it a point to sip on water, clear broths, or electrolyte drinks all day long.
- Fuel Up: Your body needs good fuel for its repair work. Focus on getting enough protein and healthy carbs.
When you're dealing with the general aches and pains that can come with treatment, exploring natural remedies for chronic pain can offer some welcome, non-medicinal comfort.
Addressing Hair Thinning and Skin Changes
First, the good news: carboplatin is much less likely to cause total hair loss compared to some other chemo drugs. Many people just experience some mild to moderate thinning that becomes more noticeable after a few cycles. This happens simply because hair follicles are among the fastest-dividing cells in the body, which makes them a target.
This effect is almost always temporary. Your hair will start to grow back once your treatment course is finished. In the meantime, treating your hair and scalp with a little extra TLC can help minimize the thinning.
Simple Care Tips:
- Switch to a mild shampoo and conditioner.
- Hold off on harsh chemicals like hair dye or perms.
- Use a wide-toothed comb, which is gentler than a brush.
- A shorter haircut can create the illusion of more volume and make any thinning less obvious.
You might also notice your skin becoming drier or more sensitive. Two simple habits can make a huge difference: moisturize daily with a fragrance-free lotion and be diligent about using a broad-spectrum sunscreen with at least SPF 30+. As always, keep your oncology team in the loop about any changes you notice so they can give you the best advice.
Your Blood Counts and Bone Marrow: What to Expect
One of the biggest impacts of carboplatin happens quietly, inside your bones. To really get what’s going on, it helps to think of your bone marrow as a non-stop factory. Its main job? To produce all the different types of cells that make up your blood.
Each of these cells has a critical role. Red blood cells are like tiny delivery trucks, dropping off oxygen to keep you energized. White blood cells are your personal security force, fighting off infections. And platelets? They're the emergency repair crew, rushing to form clots and stop bleeding.
Carboplatin is a powerful drug designed to attack fast-growing cancer cells. The catch is, it isn't always perfect at telling the difference between a cancer cell and other healthy cells that also divide quickly. Because your bone marrow factory is constantly churning out new blood cells, it can get caught in the crossfire. The result is a temporary slowdown in production, a side effect we call bone marrow suppression, or myelosuppression.
Making Sense of Your Lab Reports
This is exactly why we keep such a close eye on your blood work. Those regular blood tests, called a Complete Blood Count (CBC), are like a daily inventory report from your body’s factory. When production dips, the number of these key "workers" in your bloodstream drops, leading to a few specific conditions we watch for.
Anemia (Low Red Blood Cells): When you're short on oxygen-carrying red blood cells, you can feel wiped out, weak, and short of breath. This is the main reason behind the deep fatigue many people feel during chemo.
Neutropenia (Low White Blood Cells): Neutrophils are a special type of white blood cell—they're the first responders when an infection tries to take hold. When their numbers are low, your defenses are down, making you more likely to get sick.
Thrombocytopenia (Low Platelets): With fewer platelets on hand, your blood can’t clot as well as it normally would. You might notice you bruise like a peach or that small cuts just don't want to stop bleeding. Sometimes, it can cause nosebleeds or bleeding gums.
Myelosuppression is the most common reason we might need to adjust your carboplatin treatment. In other words, how your blood counts are doing is the main factor that guides your dose and schedule, ensuring your body has enough time to bounce back between cycles.
The numbers show just how common this is. For instance, severe thrombocytopenia (low platelets) can affect up to 66% of patients receiving carboplatin as part of a combination therapy. Neutropenia (low white blood cells) is even more common, potentially impacting up to 96% of patients. This translates to a real-world infection risk of around 16% and a bleeding risk of 8%, with 35-44% of patients needing transfusions. You can find more of this data in detailed clinical reviews.
The "Nadir" and Your Treatment Timeline
The slowdown in your bone marrow factory isn't immediate. Your blood counts will drift downward after an infusion, hitting their lowest point before starting to climb back up. In the world of oncology, we call this low point the nadir.
For carboplatin, the nadir for your platelets and white blood cells usually hits around day 21 after treatment. Knowing this timeline is key to keeping you safe. It’s why your oncologist schedules your chemo cycles with a deliberate rhythm, typically every three or four weeks.
This schedule gives your bone marrow the time it needs to recover and get production back to a safe level before the next round. If your counts are still too low, your doctor might delay treatment or lower the dose. Don't worry—this isn't a setback. It's a standard and smart safety measure to protect your health. For those curious about how doctors get a direct look at bone marrow health, you can learn more about bone marrow biopsy procedures in our guide.
Staying on top of these blood-related side effects is fundamental to good cancer care. By understanding what’s happening in your body, you can see why those regular blood tests are so important and why your treatment schedule is so carefully planned. It’s all part of the partnership between you and your care team to fight the cancer effectively while keeping you as safe and strong as possible.
Less Common Side Effects You Should Know About
While we spend a lot of time preparing for the more common challenges like fatigue and blood count dips, carboplatin can also cause a few other issues. These are less frequent, but knowing what to look for is just as important. Think of them as quieter signals from your body that tell us how you're handling the treatment.
Catching these signs early is the whole game. A quick mention to your oncology team about something new you're feeling can often lead to a simple fix, preventing a minor issue from becoming a major roadblock in your treatment.
The infographic below illustrates how carboplatin can affect your bone marrow, the factory for your blood cells. This is the root cause of the more common side effects like anemia and low platelets.
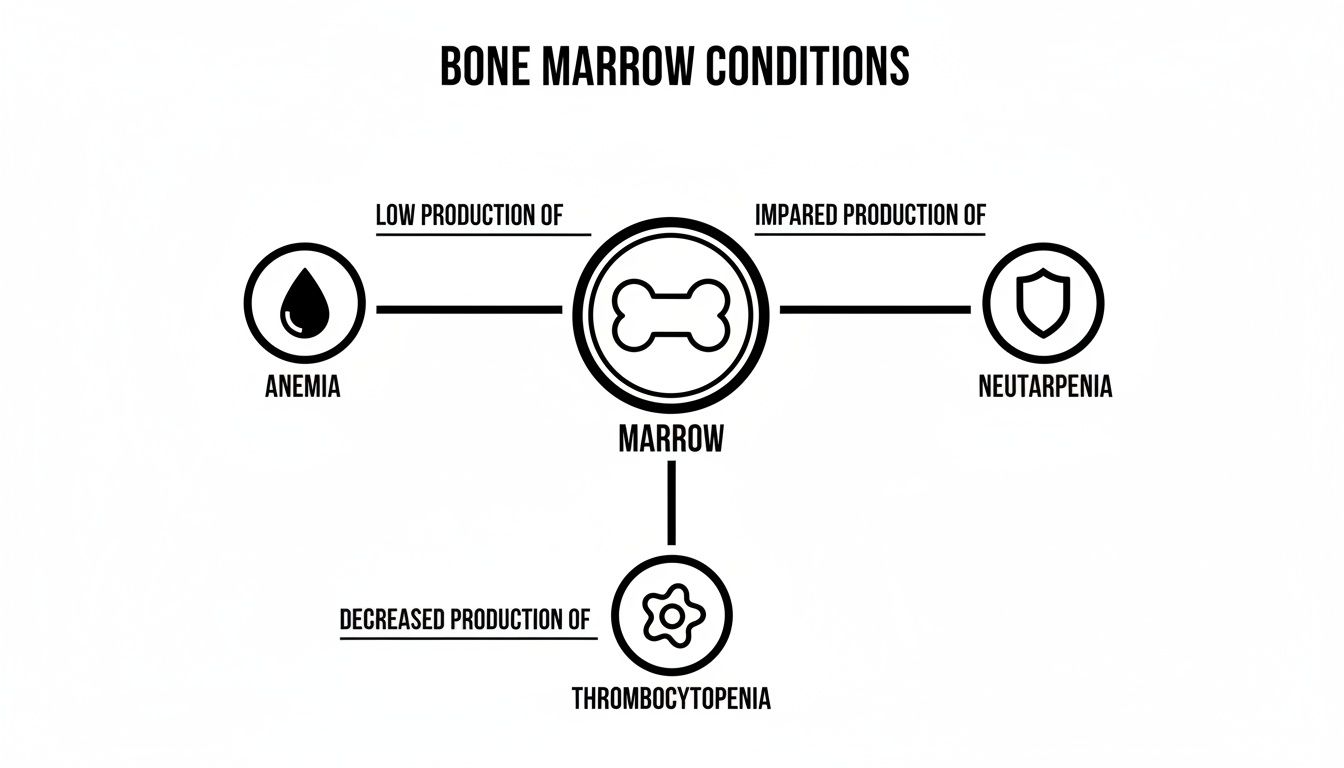
As you can see, when the bone marrow slows down, it produces fewer red cells, white cells, and platelets. Each of these dips causes specific symptoms that your team is constantly tracking.
Watching for Nerve and Kidney Changes
One of the most important, though less common, side effects to be aware of is peripheral neuropathy. This is essentially nerve irritation that tends to pop up in your hands and feet.
Imagine the nerves in your fingers and toes are like delicate wiring. Carboplatin can sometimes disrupt their signals, leading to strange sensations like:
- Tingling or a "pins and needles" feeling
- Numbness that makes it tough to do things like button a shirt or feel the floor beneath your feet
- Sharp, shooting, or burning pains that come and go
These feelings tend to creep up slowly over several cycles of treatment. The minute you notice anything like this, let your doctor or nurse know. Often, a small adjustment to your dose is all it takes to keep the neuropathy from getting any worse.
Now, carboplatin is known for being much gentler on the kidneys than its older cousin, cisplatin. That said, your team will still keep a close eye on your kidney function through regular blood work. The best thing you can do to help? Stay well-hydrated before, during, and after your infusions.
Changes in Hearing and Vision
Even more rarely, carboplatin can affect the nerves involved in hearing. The most common sign of this is tinnitus—a persistent ringing or buzzing in the ears. In very few cases, some people might notice a bit of hearing loss.
Vision changes, like blurriness, are also possible but uncommon. As with neuropathy, these aren't reasons to panic, but they are absolutely reasons to speak up. Reporting them early gives your team the information they need to manage your care effectively.
The goal of monitoring isn't just to find problems, but to get ahead of them. By keeping a close watch on these less common effects, your care team can step in early, ensuring your treatment is both effective and as comfortable as possible.
Understanding Hypersensitivity Reactions
It’s possible, though quite rare, to have an allergic-type response, known as a hypersensitivity reaction, to carboplatin. This is most likely to occur while the drug is being infused, which is precisely why our expert oncology nurses monitor you so closely during your appointment.
Symptoms can be mild or more serious and might include:
- A sudden skin rash, flushing, or hives
- Itching
- Shortness of breath or wheezing
- A drop in blood pressure, which might make you feel dizzy
- Swelling, especially around the face or throat
Your infusion team is highly trained and fully prepared to manage a reaction on the spot. They have medications ready that can stop it immediately, keeping you safe.
The risk for a reaction can go up after you've had several cycles of treatment. Some studies show the overall risk can climb to between 12-16%, though about half of these are mild. Interestingly, one trial found that using a slower, extended-infusion method dramatically cut the reaction rate from 40% to just 24.2%.
If this is a concern for you, talk to your oncologist about the specific protocols they have in place to minimize this risk. You can also learn more about symptoms of a serious reaction from the Mayo Clinic for additional information.
Taking Charge: How to Proactively Manage Your Side Effects

Managing the side effects of carboplatin is a team effort, and you are the most important person on that team. While your oncologist and nurses are the experts in medicine, you are the expert on your own body. Your daily observations and actions are what turn a standard treatment plan into one that truly works for you.
Taking a proactive role means you can significantly improve your quality of life during chemotherapy. It's about more than just taking your medications; it’s about listening to your body, knowing which signals are normal, and understanding exactly when it's time to pick up the phone. Open, honest communication is the key to a smoother and safer treatment journey.
When to Call Your Oncology Team Immediately
Some symptoms are true red flags that your body is raising, and they require urgent attention. Don't ever wait for your next scheduled appointment if you experience any of these—call your clinic’s on-call number right away, even if it's after hours or on a weekend.
- Fever: A temperature of 100.4°F (38°C) or higher is a big deal. It can be the very first sign of a serious infection, especially when your white blood cell counts are low.
- Shaking Chills: Uncontrollable shaking is a serious signal, whether you have a fever or not.
- Breathing Difficulties: Any new or worsening shortness of breath, wheezing, or feeling like you just can't catch your breath needs an immediate call.
- Signs of a Reaction: During or after an infusion, be alert for rash, hives, swelling in your face or throat, or sudden dizziness.
- Uncontrolled Bleeding: This includes nosebleeds that won’t stop after applying pressure, unusual bruising that appears without injury, or any blood in your stool or urine.
- Severe Nausea or Vomiting: If you’re at a point where you can't keep any liquids down for more than 24 hours, your team needs to know.
Your oncology team has a 24/7 line for urgent issues for a reason. It is always, always better to call and be told it's nothing to worry about than to wait and let a manageable problem become a dangerous one.
A cornerstone of proactive care is good healthcare-associated infection prevention, especially when your immune system is down. Simple things like diligent hand washing by you and your visitors can make a huge difference.
Practical At-Home Strategies for Wellness
Beyond watching for urgent symptoms, there are plenty of simple, practical things you can do at home to help yourself feel better. Think of these as ways to support your body while it does the hard work of fighting cancer and healing.
Gentle Nutrition for Nausea and Energy
- Eat Small and Often: Instead of three big meals, try five or six snack-sized ones. A constantly empty stomach can make nausea worse.
- Stick to Bland Foods: Toast, crackers, rice, chicken broth, and bananas are your friends. They’re gentle on the digestive system. Now is not the time for greasy, spicy, or super-sweet foods.
- Stay Hydrated: Dehydration is a one-two punch that worsens both nausea and fatigue. Sip water, clear juices, or electrolyte drinks all day long, even when you don't feel thirsty.
Energy Conservation to Combat Fatigue
- Prioritize Your Activities: What’s the most important thing you need to do today? Figure it out, and do it when you feel your best. Let the other stuff go.
- Embrace Short Naps: A quick 20-30 minute nap can be incredibly restorative. Any longer, and you risk messing with your nighttime sleep.
- Accept Help: This is a big one. When friends and family offer to shop, cook, or clean, let them. Saving your energy for healing is one of the most productive things you can do.
Mindful Mouth Care
- Use a Soft-Bristle Toothbrush: Your gums can become sensitive, and a soft brush helps prevent irritation and bleeding.
- Rinse After Meals: A simple saltwater rinse (mix 1/4 teaspoon of salt into a glass of warm water) keeps your mouth clean without the harshness of alcohol-based mouthwashes.
By weaving these simple habits into your daily routine, you create a healing environment for your body. This proactive approach helps you and your care team work together seamlessly, giving you more control over your cancer journey and the confidence to navigate carboplatin's side effects.
A Personal Approach to Oncology Care in New York City
Going through carboplatin treatment is a journey, and you shouldn't have to walk it alone. Here at Hirschfeld Oncology, we partner with our patients across New York City to create a care plan that’s built around you. Our focus is always on balancing the power of this treatment with your personal well-being and quality of life.
The strategies we've discussed in this guide aren't just theory—they are what Dr. Hirschfeld and our team put into practice every single day. We treat the whole person, not just the cancer, using careful monitoring and proactive support to help you feel your best.
Your Partner in Advanced Cancer Treatment
Our specialty is working with patients who have advanced or complex cancers. This often means thinking outside the box, carefully adjusting dosages, and bringing in supportive therapies to get ahead of side effects before they can take hold. We are committed to providing sophisticated, modern cancer care in a compassionate setting right here in Brooklyn.
We believe that the best cancer care happens when we work together. Your voice, your comfort, and your personal goals are at the heart of every decision we make.
If you or someone you care about is facing a cancer diagnosis, let's talk. We invite you to schedule a consultation to discuss your options and see how we can become a dedicated partner on your road ahead.
Your Questions About Carboplatin, Answered
Going through cancer treatment can feel like learning a whole new language, and it’s completely normal to have a lot of questions. Here are some straightforward answers to the things we hear most often from patients about carboplatin.
How Long Do Carboplatin Side Effects Last?
The timeline for side effects really depends on the person and the specific symptom. Some effects pop up quickly and fade just as fast, while others can linger.
The most immediate side effects, like nausea or a wave of fatigue, tend to show up within a few hours or days of your infusion. The good news is that these usually get much better before you’re due for your next cycle.
The impact on your blood counts follows a more predictable pattern. We expect your counts to hit their lowest point—what we call the "nadir"—around 21 days after your infusion. After that, they start to rebound in time for your next treatment. Other side effects, like neuropathy (that tingling in your hands and feet), can be cumulative, meaning they build up over time and may stick around for months after you’ve finished treatment. We'll be keeping a close eye on all of this.
Will I Definitely Lose My Hair?
This is a huge concern for so many people, and thankfully, with carboplatin, the answer is usually no—at least not completely. While some hair thinning is possible, it’s typically much less dramatic than with other chemo drugs.
Most people on carboplatin alone just notice their hair getting a bit thinner over the course of their treatment. It really depends on your dose and if you’re getting other drugs at the same time that are tougher on hair. If this is weighing on your mind, let’s talk about options like scalp cooling—it can make a real difference for some.
It's worth remembering that everyone reacts differently. I've had patients who saw very little change and others who experienced more noticeable thinning. Your body's response will be unique to you.
Is Carboplatin Easier on the Body Than Cisplatin?
In many ways, yes. Carboplatin is often seen as the gentler cousin of cisplatin. The main reason for this is that it's known to cause significantly less kidney damage, severe nausea, and nerve issues. That’s a big plus, and it's why we often choose it.
But there's a trade-off. Carboplatin tends to have a bigger impact on your bone marrow. This means it can drop your blood cell counts lower, which puts you at a higher risk for infections or bleeding. Choosing between the two is a very deliberate decision that we make together, based on your specific cancer, your overall health, and what we’re trying to achieve with treatment.
Can I Keep Working While on Carboplatin?
Absolutely, many of our patients continue to work through their treatment, though they almost always need to make some adjustments. How well you can manage it will depend on the kind of work you do and how you feel.
The biggest hurdle for most people is fatigue. It’s real, and it can be draining. You might need to talk to your employer about a more flexible schedule, maybe working from home a few days or cutting back on hours, especially during that first week after an infusion when you feel most wiped out. The key is open communication—with your boss and with us—so we can help you find a balance that works for you without compromising your recovery.
At Hirschfeld Oncology, our goal is to give you clear information and compassionate, personalized care through every single step. To see more about our patient-first approach to cancer treatment here in New York City, feel free to explore our other resources at https://honcology.com/blog.





.png)


.png)
.png)




