One of the most common side effects we see with chemotherapy is a drop in your white blood cell count. This condition is called neutropenia, and it simply means your body is temporarily low on a specific type of white blood cell called neutrophils—your primary infection-fighters.
It can sound pretty scary, but it’s an expected and manageable part of many cancer treatments. Chemotherapy is fantastic at targeting fast-growing cancer cells, but it can’t always tell the difference between those and other healthy, fast-growing cells, like the ones in your bone marrow that create your immune system's army.
Your Body's First Responders and Chemotherapy
I often tell my patients to think of their neutrophils as the first responders of their immune system. They’re constantly patrolling, ready to swarm and neutralize any invaders like bacteria or viruses. Chemotherapy acts like a system-wide reset, which temporarily slows down the "factory"—your bone marrow—that churns out these little soldiers.
When that factory slows production, you get a low white blood cell count during chemo, leaving you with fewer defenders on duty. This is why the risk of infection goes up. It's also why your oncology team is so vigilant about monitoring your blood work. We track those numbers carefully to keep you safe through every treatment cycle. Getting familiar with what those numbers mean is the first step to feeling more in control of the process.
Demystifying the Numbers
When you look at your lab results, the key number we're watching is your Absolute Neutrophil Count, or ANC. This gives us a precise headcount of your available infection-fighting cells. To get a bigger picture of your blood health, including red cells and platelets, it can be helpful to understand what a full blood count reveals.
A normal ANC is usually anything above 1,500 cells per microliter. Once that number dips below 1,000, your infection risk starts to climb, and we’ll begin to layer in extra precautions to protect you.
The risk isn't the same for everyone; it really depends on how low your numbers go. We categorize it to know just how careful we need to be.
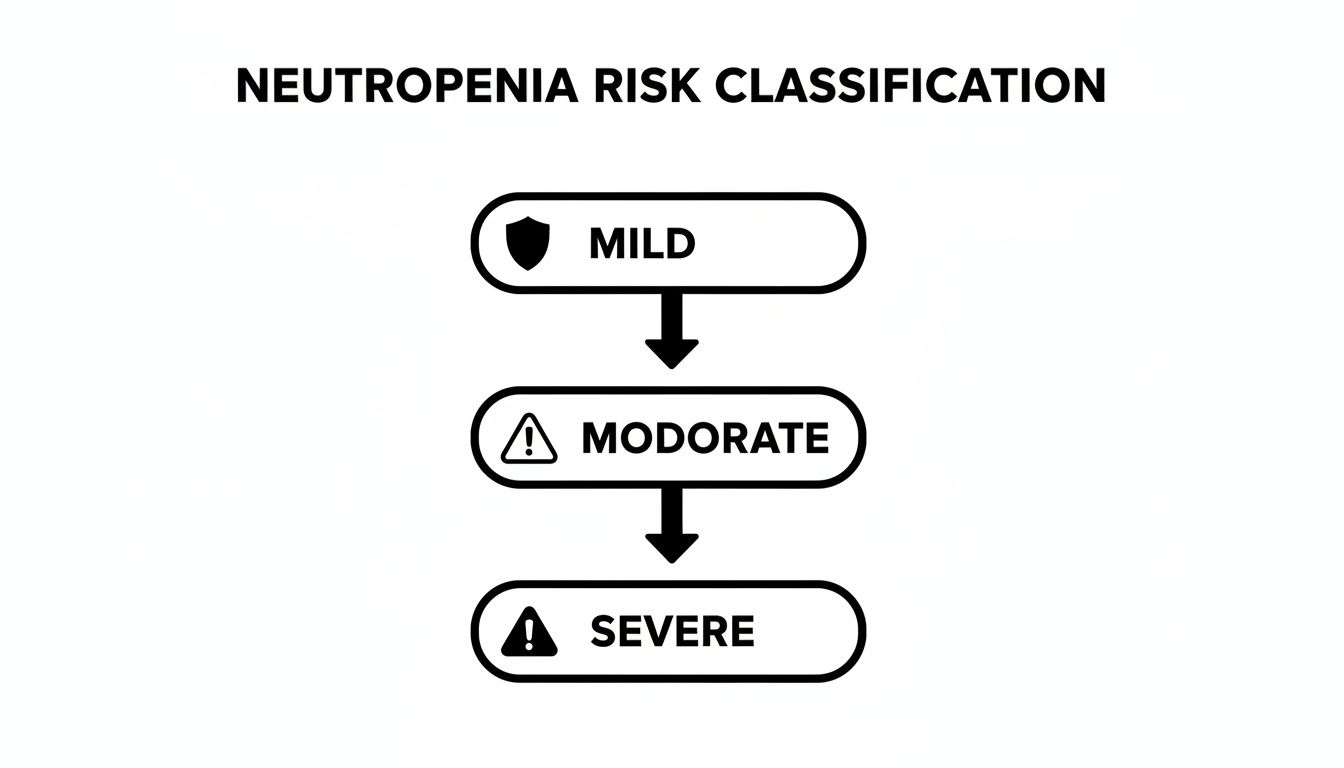
As you can see, the lower your neutrophil count falls, the more significant the risk becomes, shifting from a mild concern to a situation that requires closer medical management.
Understanding Your Neutropenia Levels at a Glance
To make it easier to talk about risk, we classify neutropenia into different "grades." This is just a simple way for the entire care team to be on the same page about how vulnerable your immune system is at any given time.
This table breaks down the different grades of neutropenia based on Absolute Neutrophil Count (ANC) to help you understand your lab results and associated risks.
Seeing your numbers fall into the moderate or severe categories doesn't mean something has gone wrong; it's often an anticipated dip. Our job is to manage it proactively with the right support to get you through it safely.
Why Chemotherapy Affects Your White Blood Cell Count
To get a handle on why chemo impacts your white blood cells, it helps to picture your bone marrow as a bustling factory. This factory works around the clock, producing all the vital components of your blood: red cells to carry oxygen, platelets to stop bleeding, and of course, white blood cells to fight off infections.
Chemotherapy drugs are powerful, designed to hunt down and destroy cells that divide rapidly—the very definition of cancer. The problem is, these drugs aren't always great at telling the difference between a cancer cell and other healthy cells that also happen to divide quickly. The cells in your bone marrow "factory" fall squarely into that category.
So, while the chemo is doing its job on the cancer, it also inadvertently slows down the production lines in your bone marrow. The cells hit hardest are the ones with the shortest lifespan, and neutrophils—your body’s most crucial infection-fighting white blood cells—are at the top of that list. This "collateral damage" is exactly why you see a low white blood cell count during chemo.
High-Risk Regimens and the Nadir Cycle
Not all chemotherapy treatments pack the same punch when it comes to neutropenia. Some drugs are simply known for being tougher on the bone marrow, a property we call myelosuppression.
Chemo regimens that are well-known for causing a significant drop in white blood cells often include:
- Anthracyclines: Drugs like doxorubicin (Adriamycin) and epirubicin, which are workhorses in treating breast cancer and sarcomas.
- Taxanes: You’ll see paclitaxel (Taxol) and docetaxel (Taxotere) used often for breast, ovarian, and lung cancers.
- Platinum-based drugs: Cisplatin and carboplatin are go-to treatments for cancers of the lung, ovaries, and bladder.
- Topoisomerase inhibitors: Etoposide and irinotecan are used for a range of cancers, including lung and colorectal.
This dip in your cell count isn’t random; it follows a predictable pattern with each treatment. Your white blood cell count usually starts to fall a few days after an infusion, hitting its lowest point about 7 to 14 days later. This low point has a specific name: the nadir. After the nadir, your bone marrow factory gets back to work, and your counts slowly recover just in time for your next treatment.
This predictable rhythm is why we time your blood tests so precisely. By knowing when to expect the nadir, your oncology team can anticipate when you’ll be most vulnerable and step in with the right support.
Why the First Cycle Is Often the Riskiest
It’s interesting—the risk of developing a serious complication like febrile neutropenia (getting a fever when your counts are dangerously low) isn’t the same for every cycle. The data consistently shows that the very first cycle of treatment is the most dangerous.
For example, a major study found that while the overall risk of febrile neutropenia was 13-21%, it shot up to 23-36% during the first cycle alone. The risk tends to go down after that because your oncologist has a chance to see how your body responds and can make adjustments, like changing a dose or adding growth factor shots to help your bone marrow recover.
This is why your care team watches you like a hawk after that first infusion. By monitoring you closely from the start, we can personalize your treatment plan to make every following cycle much safer and easier to handle. You can learn more about this process in our general guide covering what to expect during chemotherapy.
How to Recognize the Signs of an Infection
When your white blood cell count is low, you won't necessarily feel it. There isn't a specific symptom that screams "neutropenia." Instead, the real sign is what happens when your body can't fight off germs it normally would. Your main job becomes spotting the earliest hints of an infection before it has a chance to gain a foothold.
Think of your immune system's first responders being on leave. A tiny spark that would normally be extinguished immediately can now turn into a serious fire. That's why learning to recognize the subtle clues of an infection is one of the most critical skills you'll develop during your treatment. It's about shifting your mindset to be incredibly in tune with any new changes in how you feel.
This kind of awareness is empowering. It helps you and your care team get ahead of any problems, ensuring you get the right support exactly when you need it most.
Fever: The Most Critical Warning Sign
During chemotherapy, a fever isn't just a fever—it's a full-blown emergency signal. When you have a fever combined with a low white blood cell count, it's a condition called febrile neutropenia, and it demands immediate medical attention. It's the most reliable sign that your body is battling an infection without a full army.
Your oncology team will give you a very specific temperature that should trigger an immediate phone call, no matter the time of day or night. Usually, that threshold is a single temperature reading of 101°F (38.3°C) or a temperature that stays at 100.4°F (38°C) for an hour or more.
You have to take this seriously. Never just assume a low-grade fever will resolve on its own, especially when you're in that high-risk nadir period.
A Warning About Fever-Reducing Medications: Be very careful with over-the-counter fever reducers like acetaminophen (Tylenol) or ibuprofen (Advil, Motrin). Do not take them to bring down a fever unless your oncologist has specifically told you it's okay. These drugs can mask this critical warning sign and delay the urgent care you need.
Your Daily Self-Monitoring Checklist
Beyond checking your temperature, it’s a great idea to get into the habit of doing a quick daily check-in with your body. Be on the lookout for anything new or different that could point to an infection just starting to brew.
Here’s a quick rundown of red flags that should prompt a call to your care team:
- Chills, Shaking, or Sweats: These often go hand-in-hand with a fever and are a clear sign your body is trying to fight something off.
- New Cough or Shortness of Breath: Could be a sign of a respiratory infection like pneumonia, which needs to be addressed quickly when you're neutropenic.
- Sore Throat or Painful Swallowing: A brand-new, sharp sore throat can signal a local infection.
- Mouth Sores or White Patches: Take a look inside your mouth for any new sores, redness, or white spots, which can be a sign of a fungal infection like thrush.
- Burning or Pain When You Urinate: This is the classic tell-tale sign of a urinary tract infection (UTI).
- Redness, Swelling, or Pain on Your Skin: Pay extra attention to your skin, especially around any cuts, surgical wounds, or near your port or catheter site.
- New Abdominal Pain or Diarrhea: While these can certainly be side effects of chemo, if they're new or unusually severe, they could also indicate a gastrointestinal infection.
- Unusual Vaginal Discharge or Itching: This could signal a yeast infection or another localized infection.
This checklist is here to empower you, not to make you anxious. When you know exactly what to look for, you can turn that feeling of uncertainty into confident action. You become an active partner in your own care, ready to spot potential issues at their earliest—and most treatable—stage.
Knowing what to look for is your best defense. The table below summarizes the most critical symptoms that mean you need to get in touch with your care team right away.
Red Flag Symptoms When Your White Blood Count Is Low
Remember, your oncology team wants to hear from you. It is always better to call about a symptom that turns out to be nothing than to wait on something that turns out to be serious. Your vigilance is a crucial part of keeping you safe during treatment.
How We Medically Manage Low White Blood Cell Counts

When your lab results show a drop in white blood cells during chemo, it's a signal for your oncology team to step in with support. This isn't a sign that your treatment is failing—far from it. It’s an expected side effect that we are fully prepared to manage. Our goal is always to keep your treatment on schedule while minimizing your infection risk, and we have several effective tools to do just that.
The most common approach involves medications that kick-start your bone marrow, helping it recover and produce new neutrophils more quickly. Think of these treatments as giving your body's internal "factory" a much-needed boost, ensuring your immune defenses don't stay down for long.
Boosting Production with Growth Factors
One of the cornerstones of managing neutropenia is a class of drugs called Granulocyte-Colony Stimulating Factors (G-CSFs). These are biologic medications that essentially act like a supervisor for your bone marrow, telling it to ramp up the production of granulocytes, which include those all-important neutrophils.
You might hear us refer to them by their brand names:
- Pegfilgrastim (Neulasta): This is a long-acting injection, usually given as a single shot about 24 hours after your chemo infusion. It’s designed to work its magic throughout your entire nadir period.
- Filgrastim (Neupogen): This is the short-acting version, which requires a series of daily injections for several days after chemo.
These "growth factor" shots are incredibly effective at making neutropenia less severe and shortening how long it lasts. By reducing the time your immune system is vulnerable, they significantly lower your risk of developing a serious infection or febrile neutropenia, which can land you in the hospital.
We often use G-CSFs as a primary prevention strategy. If your chemotherapy regimen has a high risk—over a 20% chance—of causing febrile neutropenia, your oncologist will likely prescribe these shots right from your very first cycle.
Tailoring Your Treatment Plan
Besides stimulating new cell growth, your oncology team has other ways to handle a low white blood cell count. The approach we take is always personalized, balancing the need to attack the cancer with the absolute priority of keeping you safe.
One common strategy is chemotherapy dose modification. If your counts are too low to proceed safely with your next treatment, your oncologist might suggest delaying your infusion for a week. This pause gives your bone marrow a little extra time to recover on its own. In some cases, we might also decide to reduce the dosage of your chemotherapy drugs in future cycles to lessen the impact on your bone marrow while maintaining the treatment's effectiveness.
This kind of adjustment is a normal part of the process and reflects a careful, responsive approach to your care.
Using Antibiotics to Prevent Infection
In certain high-risk situations, your doctor might prescribe prophylactic antibiotics. This simply means you would take an antibiotic to prevent an infection from ever starting, rather than waiting to treat one after it appears.
This is typically reserved for patients who we expect will have severe and prolonged neutropenia (an ANC below 500 for more than seven days). By taking a preventative antibiotic, you can help shield yourself from common bacterial invaders during your most vulnerable window.
Chemotherapy-induced neutropenia is a serious issue in cancer care. In the United States, hospitalization rates for neutropenia reach 7.83 cases per 1,000 cancer patients. While some studies suggest febrile neutropenia affects 13-21% of patients with solid tumors, real-world data shows this figure can be much higher, which is why these medical interventions are so important. If you're interested in the broader impact, you can read more about chemotherapy-induced neutropenia epidemiology forecasts.
Practical Ways to Prevent Infection at Home
While your medical team has a plan for managing a low white blood cell count, what you do at home is just as crucial. When your immune defenses are down, your everyday world presents a whole new set of challenges. The good news is that simple, consistent habits are your most powerful allies for staying healthy between treatments.
Think of it as shoring up the defenses of your own personal space. You’re creating a safe harbor where germs have a much harder time getting in. This doesn't mean you need to live in a sterile bubble, but it does mean being more mindful of hygiene, how you handle food, and your daily interactions. These small adjustments can make a huge difference in your risk of infection.
Mastering Personal Hygiene
The single most effective tool in your infection-prevention toolbox is also the simplest: excellent handwashing. Our hands touch countless surfaces all day long, making them the number one carrier for germs. When your neutrophils are low, this basic habit becomes your absolute first line of defense.
- Wash Often and Well: Lather up with soap and warm water for at least 20 seconds—the time it takes to hum "Happy Birthday" twice through. Make it a routine before you eat, after using the restroom, after petting your animals, and as soon as you get home from an outing.
- Encourage Others: Don't feel awkward about asking family and visitors to wash their hands when they arrive. Just explain it's a simple way they can help keep you safe.
- Use Hand Sanitizer: When you can't get to a sink, an alcohol-based hand sanitizer with at least 60% alcohol is the next best thing.
Beyond your hands, keeping your body's other natural barriers—your skin and mouth—in good shape is also key. Tiny breaks in the skin or irritation in your mouth can become easy entry points for bacteria.
Taking care of your mouth and skin is more than just about comfort; it's a core part of your infection prevention plan. Healthy skin and a healthy mouth are formidable shields against bacteria that can cause serious trouble when you're neutropenic.
Use a soft-bristle toothbrush so you don't irritate your gums. It's also a good idea to check with your oncology team before using mouthwash, as some formulas can be too harsh. For your skin, a daily habit of using a gentle, unscented lotion will help prevent the kind of dryness and cracking that can let germs in, especially right after a shower.
Creating a Safe Food Environment
Your kitchen needs a little extra attention when your white blood cell count is low. Foodborne illnesses that a healthy immune system would shrug off can become a serious threat. The mission here is to stop potential bacteria before they ever make it to your plate.
This really comes down to being meticulous about how you choose and prepare your food. For a deeper dive, check out our guide on what to eat during chemotherapy, which has even more advice on nutrition and food safety.
Here are the non-negotiable rules for food safety:
- Cook Foods Thoroughly: Make sure all meat, poultry, fish, and eggs are cooked to the proper internal temperature. This isn't the time for raw or undercooked foods like sushi, raw oysters, or runny eggs.
- Wash All Produce: Every fruit and vegetable needs a good rinse under running water, even if you’re going to peel it. Bacteria on the peel can easily transfer to the flesh when you start cutting.
- Avoid High-Risk Foods: It's best to steer clear of things like unpasteurized dairy products (think soft cheeses), deli meats, and anything from a salad bar or buffet where the risk of contamination is higher.
Navigating Daily Life and Your Home
Managing your environment goes beyond the kitchen sink. It’s about making smart, conscious choices about your daily activities and who you're around, especially during that low-point in your chemo cycle, the nadir.
In Your Home:
- Pet Care: You can absolutely still snuggle with your furry friends! Just have someone else handle cleaning the litter box or picking up animal waste. If you must do it yourself, wear disposable gloves and wash your hands thoroughly right after. And as tempting as it is, try to avoid letting pets lick your face or near any open cuts.
- Gardening and Yard Work: Digging in the dirt can expose you to fungi and bacteria in the soil, so it's best to take a break from gardening. If you can't resist, be sure to wear gloves and a mask.
- Cleaning: Give high-touch surfaces like doorknobs, light switches, and remote controls a regular wipe-down with a disinfectant. For more general tips on keeping your home a healthier space, this is a practical guide on how to prevent virus infection.
Outside Your Home:
- Avoid Crowds: When your counts are at their lowest, try to skip crowded indoor places like malls, movie theaters, or buses and trains.
- Mask Up: A well-fitting mask is an excellent layer of protection when you're in public indoor settings.
- Be Mindful of Sick Contacts: Ask friends and family to please wait to visit if they're feeling unwell, even if it's "just a cold." It's a small request that makes a big difference.
When to Call Your Doctor Immediately

This is perhaps the most important thing you'll learn about managing chemo side effects: knowing when to pick up the phone. Some issues can be managed at home, but others are true medical emergencies. When your white blood cell count is low, there’s no room for a "wait and see" attitude. You have to be proactive.
The biggest red flag—the one that requires you to act without delay—is a fever. When your neutrophil counts are down, a fever is a big deal. We call this febrile neutropenia, and it is always treated as an emergency. Your oncology team has a 24/7 on-call number for this very reason.
Here’s the hard-and-fast rule: call your care team immediately if you get a single temperature reading of 100.4°F (38°C) or higher. Don’t talk yourself out of it. Don't wait to see if it comes down. It doesn't matter if it's 2 a.m. on a Sunday—this is exactly what the on-call service is for.
What to Expect When You Call
When you call, the nurse or doctor on the line will need a few key details. Be ready to tell them your temperature, when your last chemo infusion was, and if you’re feeling anything else, like chills, a new cough, or pain anywhere.
Based on that conversation, the advice will almost certainly be the same: you need to go to the emergency room. In most cases, your oncology team will call the ER ahead of time to give them a heads-up that you're on your way and explain your situation.
Remember, a fever in a neutropenic patient is considered an infection until proven otherwise. The whole goal is to get you started on treatment right away, because a simple infection can spiral into something serious very quickly when you don't have enough white blood cells to fight it.
Heading to the hospital is never fun, but knowing the game plan can make a stressful situation feel a little more manageable. This process is designed to be fast and thorough to keep you safe.
At the Emergency Room
The moment you arrive, tell the check-in staff that you are a chemotherapy patient with a fever. This simple phrase is your fast-pass; it lets them know to prioritize your care. They'll likely give you a mask and get you into a private room as soon as one is available to shield you from any germs in the waiting area.
Once you’re settled, the medical team will get to work trying to pinpoint the source of the infection. This usually involves a standard set of tests:
- Blood Cultures: They’ll draw blood from two different spots to check for any bacteria in your bloodstream. This is the most crucial test for finding a serious infection.
- Complete Blood Count (CBC): This lab work confirms your exact white blood cell and neutrophil levels.
- Chest X-ray: This is a quick way to look for any signs of pneumonia.
- Urine Sample: This helps rule out a urinary tract infection (UTI), a common culprit.
You won't have to wait for the results to come back before treatment begins. The team will almost immediately start you on broad-spectrum intravenous (IV) antibiotics. Think of these as the heavy hitters—powerful antibiotics that target a wide range of bacteria. Time is of the essence, so they get them started right away. The specific side effects you experience can vary based on your chemo regimen; for more details, you can read our guide on 5-Fluorouracil side effects.
It's very common for patients with febrile neutropenia to be admitted to the hospital for a few days. This allows the team to continue the IV antibiotics and keep a close eye on you until the fever breaks and your neutrophil counts start to bounce back. It might feel like an annoying detour in your treatment journey, but it’s the absolute safest way to handle a serious complication and get you back on track.
Your Top Questions About Neutropenia, Answered
When you're dealing with a low white blood cell count during chemo, a lot of practical, day-to-day questions pop up. Let's tackle some of the most common things patients ask about.
Is There a Special Diet to Boost My White Blood Cells?
This is a great question, and one we hear all the time. While eating well is absolutely crucial for keeping your strength up during chemo, unfortunately, there’s no magic food that can single-handedly raise your white blood cell count. Chemotherapy's effect on your bone marrow is just too strong for diet to overcome it alone.
Instead of focusing on boosting your counts with food, shift your focus to food safety. This means cooking food thoroughly, scrubbing your fruits and vegetables, and steering clear of higher-risk items like sushi or unpasteurized cheese. The real heavy lifting for stimulating white blood cell production comes from medical treatments your oncologist prescribes, like G-CSF shots.
How Long Does Neutropenia Actually Last?
Thankfully, the timeline for neutropenia is usually pretty predictable. Your white blood cell count will typically hit its lowest point, what we call the nadir, about 7 to 14 days after your chemo infusion. The exact timing can vary a bit depending on the specific drugs you're receiving.
After this dip, your body naturally starts to rebuild its supply of white blood cells in time for your next treatment. We keep a close eye on this cycle with regular blood tests and will step in if your body needs a little more time or support to recover.
Knowing this rhythm is incredibly helpful. It tells you exactly when to be extra vigilant—that one- to two-week window after treatment is when you’re most vulnerable and need to be most careful about preventing infection.
Can I Still Have Friends and Family Over?
Yes, absolutely! Having your support system around is so important. You just need to set a few ground rules to keep you safe. The number one rule is simple: if someone feels sick, even with just a sniffle or a slight cough, they need to wait until they're better to visit.
When visitors arrive, have them wash their hands well right away. It's also a good idea to skip big crowds and maybe keep a bit of distance from anyone who's been sick recently, especially when you're in that nadir period.
Will My Counts Drop This Low After Every Single Treatment?
Not always. The first round of chemo often poses the biggest risk for a steep drop in your white blood cells. It's the first time your body is experiencing these drugs, so we're all learning how you’ll react.
Based on how you do after that first cycle, we might adjust the plan. We might add a growth factor shot to help your bone marrow, tweak your chemo dose, or push your next treatment back a few days to give you more recovery time. We make these changes proactively to make every following cycle safer and easier on you.
At Hirschfeld Oncology, we know that managing treatment safely is all about proactive care and open communication. If you have more questions or are looking for a personalized cancer care plan in the New York City area, we're here to help. You can request a consultation and learn more about our patient-first approach.





.png)


.png)
.png)




